What Is Contact Dermatitis?
What Is Contact Dermatitis?
Dermatitis, also known as skin inflammation or irritation, is a condition that causes discomfort and itchiness. Contact dermatitis, a specific type of dermatitis, occurs when the skin reacts to allergens or irritants, resulting in painful and/or itchy rashes. This condition can be triggered by contact with substances like poison ivy (known as allergic contact dermatitis) or chemical solvents (known as irritant contact dermatitis). While irritant contact dermatitis can occur after a single exposure or repeated exposure to the irritant, allergic contact dermatitis requires multiple exposures to develop an allergy. As a result, individuals in certain professions, including construction workers, florists, food workers, hair stylists, healthcare professionals, artists, janitors, plumbers, and mechanics, are at a higher risk of developing contact dermatitis compared to others.
Contact Dermatitis Symptoms
Contact dermatitis typically presents with initial symptoms of itchy and uncomfortable red skin, which is then followed by the appearance of a rash. In some cases, blisters may also develop in the affected area. It is important to note that contact dermatitis is not contagious, meaning it cannot be transmitted to others. Due to the wide range of substances that can irritate the skin or trigger an allergic reaction, contact dermatitis is a common reason why patients seek appointments with dermatologists. The specific symptoms experienced can vary depending on the cause of the dermatitis and an individual’s sensitivity to the triggering substance.
Allergic contact dermatitis can manifest with various symptoms, including:
- Skin redness: The affected area may appear reddened or flushed.
- Darkened or leather-like skin: Prolonged inflammation can cause the skin to darken or become thick and leathery.
- Dry, scaly, and flaky skin: The skin may become dry, rough, and develop flakes or scales.
- Hives: Raised, itchy welts or bumps known as hives may appear on the skin.
- Oozing blisters: In severe cases, the skin may develop blisters that ooze fluid.
- Burning sensation: The affected area may feel a burning or stinging sensation.
- Extreme itchiness: Itching is a common symptom of contact dermatitis and can be intense.
- Sensitivity to sunlight: Some individuals may experience increased sensitivity to sunlight in the affected area.
- Swelling: The skin may become swollen, especially in the area of contact with the allergen.
It is important to note that not all individuals will experience all of these symptoms, and the severity of symptoms can vary from person to person.
Allergic contact dermatitis is a type of eczema that causes itchy, red, irritated skin. Its first sign is often itchy skin, followed by a rash and possibly blisters. You can get allergic contact dermatitis when things you touch, or that touch you, annoy or irritate your skin. Did you know that more than 15,000 things that touch our skin can cause an allergic reaction—including fragrances and nickel?
In some cases, people get contact dermatitis when the sun hits their skin. The American Academy of Dermatology gives this example: a bartender may squeeze lemons and limes while indoors and never develop a rash. However, when they squeeze lemons and limes outdoors on a sunny day, a painful rash and large blisters develop where the sunlight hits the skin coated with juices.
Contact dermatitis is not contagious.
Rashes have the potential to manifest on any part of the body due to a multitude of factors. One of the prevalent skin conditions, known as contact dermatitis, is neither contagious nor life-threatening, but it can cause significant discomfort. In certain instances, seeking assistance from a dermatologist in Poughkeepsie NY, Fishkill NY, or New Milford CT becomes necessary to effectively alleviate symptoms. At The Art of Skin Dermatology we provide comprehensive and clinical treatments for a range of skin conditions, including contact dermatitis. Reach out to our experienced dermatologists today to schedule an appointment and discover the array of treatments we offer.
Irritant Contact Dermatitis
Irritant contact dermatitis can present with several symptoms, including:
- Blistering skin: The affected area may develop blisters filled with fluid.
- Cracked skin: The skin may become dry and cracked, leading to discomfort and potential pain.
- Extreme dryness: The skin may become excessively dry, resulting in flakiness and roughness.
- Swelling: The affected area may become swollen, causing discomfort and a change in appearance.
- Tight or stiff skin: The skin may feel tight or stiff, limiting movement and causing discomfort.
- Open sores with crusts: In severe cases, the skin may develop open sores that form crusts.
- Ulcerations: Deep, painful sores or ulcers may develop in the affected area.
It is important to note that the severity and combination of symptoms can vary depending on the individual and the specific irritant involved. Prompt identification and avoidance of the irritant are crucial for managing and treating irritant contact dermatitis.
Contact Dermatitis Causes
There are three common types of dermatitis: allergic contact dermatitis, irritant contact dermatitis, and photocontact dermatitis.
Photocontact dermatitis is a less common type of dermatitis that occurs when an active ingredient in a skincare product reacts with sunlight, leading to skin irritation. This reaction can cause symptoms such as redness, itching, and inflammation.
Allergic contact dermatitis happens when the skin develops an allergic reaction after exposure to a foreign substance. This exposure triggers the release of inflammatory chemicals in the body, resulting in itchy, inflamed, and irritated skin. Common causes of allergic contact dermatitis include plants like poison oak or poison ivy, latex, perfumes, formaldehyde, Balsam of Peru, certain medications, cosmetics, and jewelry made with nickel or gold, among other allergens.
Irritant contact dermatitis is the most common type of contact dermatitis. It occurs when the skin comes into contact with a toxic substance. These substances can include bleach, drain cleaners, rubbing alcohol, airborne irritants, fertilizers, pesticides, kerosene, detergents, pepper spray, battery acid, and more. Overexposure to less irritating substances like soap or water can also lead to irritant contact dermatitis. Certain professions, such as hairstyling, bartending, and healthcare, where frequent exposure to water is common, can increase the risk of developing irritant contact dermatitis on the hands.
How Long Does Contact Dermatitis Last?
Contact dermatitis typically occurs on the areas of the body that have direct contact with the substance causing the reaction. For example, if you brush against poison ivy, the rash is likely to develop on the limb that came into contact with the plant. Similarly, if you have pierced ears and wear earrings made with nickel, the dermatitis may occur around the pierced area.
The rash usually appears within minutes to hours after exposure to the irritant or allergen and can last for a duration of 2 to 4 weeks. In cases of chronic exposure to a mild irritant like water or soap, the reaction may occur over a prolonged period of weeks to months, with symptoms typically appearing on the hands.
While allergic contact dermatitis can initially be limited to the site of contact, it often spreads beyond the original area. This means that the rash may extend beyond the point of contact and affect surrounding skin.
It is important to note that the specific pattern and extent of the rash can vary depending on the individual, the sensitivity to the substance, and the duration and intensity of exposure.
How Can I Prevent Contact Dermatitis?
These are excellent tips recommended by dermatology associates to help prevent symptoms associated with contact dermatitis. Here is a summary of the tips:
- Identify and avoid irritants and allergens: Be aware of substances that may trigger a reaction and try to avoid them.
- Wash your skin after contact: If you come into contact with an irritant or allergen, wash your skin thoroughly to remove it.
- Apply and reapply sun protection: Protect your skin from the sun by applying sunscreen regularly.
- Wear protective clothing or gloves: Use protective clothing or gloves when handling substances that may cause a reaction.
- Cover metal fasteners: If you have metal fasteners on clothing that may cause a reaction, cover them with iron-on patches.
- Apply a barrier cream or gel: Use a barrier cream or gel to create a protective layer on your skin.
- Use natural moisturizers: Opt for natural moisturizers that are less likely to contain irritants or allergens.
- Take care around pets: Be cautious if you have allergies to pet dander or saliva, and take appropriate measures to minimize exposure.
- Purchase dermatologist-recommended skin care 9. Purchase dermatologist-recommended skin care: Choose skincare products that are recommended by dermatologists, as they are more likely to be formulated with gentle ingredients and be suitable for sensitive skin.
- Stick with “hypoallergenic” and “unscented” products: Look for products labeled as “hypoallergenic” and “unscented,” as these are less likely to contain common irritants or allergens.
- Opt for wearing vinyl gloves instead of latex gloves: If you have a latex allergy, choose vinyl gloves as an alternative to avoid triggering a reaction.
- Wear long-sleeved shirts and pants while outdoors: When spending time outdoors, especially in areas with potential irritants or allergens, cover your skin with long-sleeved shirts and pants to minimize exposure.
- If a product causes irritation, stop using it immediately: If you notice any signs of irritation or a rash after using a particular product, discontinue its use right away to prevent further aggravation.
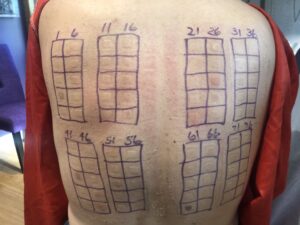
- Always do spot tests of new products on your forearm: Before using a new product on a larger area of your skin, perform a spot test by applying a small amount on your forearm and monitoring for any adverse reactions.
By following these tips, you can reduce your risk of contact dermatitis and minimize the occurrence of symptoms. However, if you experience persistent or severe symptoms, it is important to consult with a dermatologist for proper diagnosis and treatment.

 What Is Contact Dermatitis?
What Is Contact Dermatitis?